Specialty and New Pharmaceutical Product Launches Might be Negatively Impacted if Appropriate Support is Not built-in to Assist Patients with Complex Care. Healthcare Providers (HCPs) are Not Always Best Equipped to Navigate this Growing Burden.
$40.6 billion is spent annually on processing patient insurance benefit verification including prior authorizations (PAs) and out-of-pocket maximums, primary and secondary insurance coverage, cost- sharing, and submitting claims as well as any follow-ups for denials, appeals, and reimbursement 1. Healthcare providers and practice managers spend up to 31 days managing PA requests, resulting in an estimated $13.3 billion in administrative cost and burden.2
PA Burden Grows and Grows for Practice Managers
Insurers have increased the use of PAs over the past years for procedures (84%); for diagnostic tools (78%); and for prescription medications (80%) 3. Nearly 59% of physicians have staff members working exclusively on PAs, with most staff spending between 10-20 hours per week on PAs.
Impact to Patients Accessing Specialty and New Pharmaceutical Products
The prior authorization (PA) process is linked to a significant rise in prescription abandonment rates, approaching nearly 40%, which poses concerns regarding adverse health outcomes and hospitalizations, particularly in chronic disease management. While optimal therapeutic efficacy often necessitates medication adherence rates exceeding 80%, only half of patients achieve this, with PA requirements potentially exacerbating the challenge, as indicated by the perspectives of 75% of surveyed physicians. 4
PA Innovation Mandate via Federal Policy Proposal
On January 17, 2024, the Centers for Medicare and Medicaid Services (CMS) issued its final rule governing
certain prior authorization timelines and interoperability rules.5 CMS now requires most payers to
implement and maintain a Prior Authorization API that is populated with its list of covered items and
services, can identify documentation requirements for prior authorization approval, and supports a prior
authorization request and response. These Prior Authorization APIs must also communicate whether the
payer approves the prior authorization request (and the date or circumstance under which the authorization
ends), denies the prior authorization request (and a specific reason for the denial), or requests more
information. This requirement must be implemented beginning January 1, 2027.
CMS acknowledges that PAs are not going away and that the process plays a major role in health care in that
it can ensure that covered items and services are medically necessary and covered by the payer. However, at
the same time, CMS is concerned that PAs are a major source of burnout and can become a “health risk for
patients if inefficiencies in the process cause care to be delayed.” 6
Examples of inefficiencies include but are not limited to:
- HCPs expend resources on staff to identify PA requirements that vary across payers and navigate the submission and approval processes, which could otherwise direct to clinical care.
- Patients may unnecessarily pay out-of-pocket or abandon treatment altogether when PAs are delayed.
- Patients may abandon treatment for a period, go untreated, then present to their HCP in a worse condition in need of more complex care.
CMS Rule Summary:
- It focuses on improving the PA process through a mandated consistent technology interface between provider portals/EMRs and payers with an already established Patient Access Application Program Interface (API) to reduce time spent on manual activities significantly.
- It enhances the suite of APIs by building a dedicated PA Requirements, Documentation and Decision (PARDD) API that would automate the process for providers to determine whether a PA is required, identify PA information, and provide to the provider all needed documentation required, as well as facilitate the exchange of PA requests and decisions from the EMR or practice management system.
- It requires payers to send PA decisions electronically within 48-72 hours for expedited (i.e., based on urgency levels TBD) requests and 5-7 calendar days for standard (i.e., based on non-urgent levels TBD) requests so that delay in obtaining treatment is not stalled by paperwork that does not drive increases in patient outcomes.
At COPILOT, there are Innovative PA and Pre-Certification Solutions available including ePA.
With more than 12 years of industry experience, COPILOT is able to accurately navigate the evolving healthcare landscape alongside provider offices. As a trusted partner, COPILOT is ready to adapt to the industry’s imminent shift towards full automation.
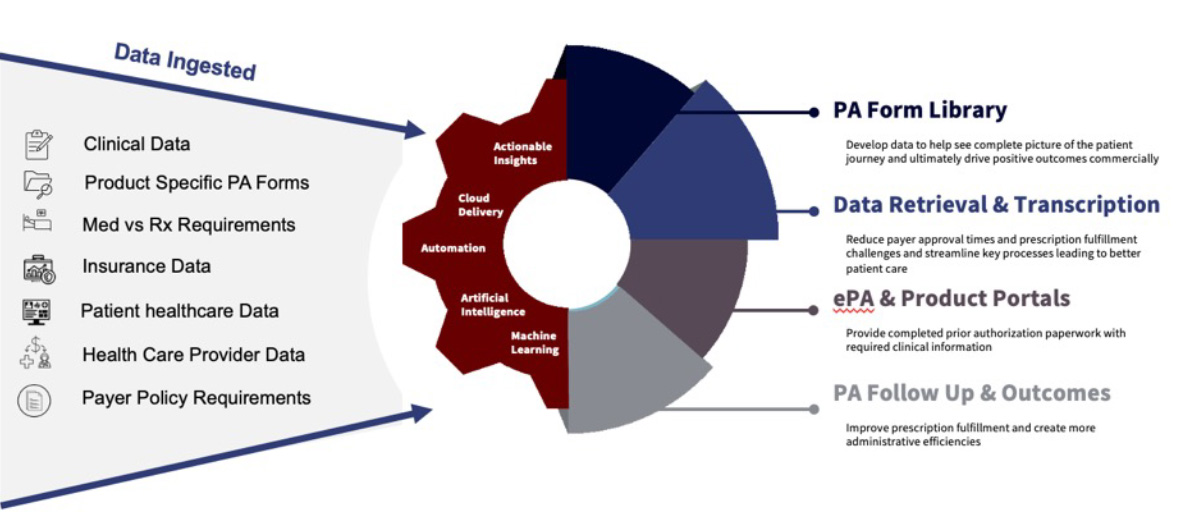
- PA/Pre-Certification Medical Benefit Online Library and API Option: COPILOT offers a digitized PA/ pre-cert form for specialty pharmaceutical products across all payers and aggregates them into a dedicated module within the HCP-facing portal, to allow HCPs and practice managers a centralized online library to search, populate, and submit PAs to payers.
- AUTOPILOT E-Services: COPILOT has a suite of APIs that includes the ability to interface its ePA solutions with EMR and practice management tools. If HCP prefers not to integrate its EMR/practice management system with AUTOPILOT, it can still securely transmit clinical information to COPILOT, which has a transcription tool that transcribes notes into the PA forms and sends them back to HCP via a secured link, portal, or the preferred workflow of the practice for submission.
- BV and PA Turnaround Time: COPILOT benefit verification results to HCPs are same day most often with a 95% same day turnaround time (TAT) for both medical and pharmacy benefit investigations. COPILOT technology enablement solutions intend to contribute to burden reduction for HCPs and practice managers by substantially automating manual tasks and decreasing the volume of denials or appeals.
Contact info@cmcopilot.com or me to schedule a Capabilities Presentation and Platform Demo.
Valerie Sullivan
Chief Commercial Officer
COPILOT
VSullivan@cmcopilot.com
- https://www.fiercehealthcare.com/practices/costs-prior-authorizations-increase-for-physician-practices-at-alarming-rate
- https://www.regrelief.org/wp-content/uploads/2019/12/RRC-Prior-Authorization-Survey-Results-FINAL-7-26.pdf
- https://www.regrelief.org/wp-content/uploads/2019/12/RRC-Prior-Authorization-Survey-Results-FINAL-7-26.pdf
- https://www.priorauthtraining.org/the-impact-of-prior-authorization-on-patient-compliance-and-adherence/
- https://www.cms.gov/newsroom/fact-sheets/cms-interoperability-and-prior-authorization-final-rule-cms-0057-f
- https://www.cms.gov/newsroom/fact-sheets/advancing-interoperability-and-improving-prior-authorization-processes-proposed-rule-cms-0057-p-fact
Download